Before we get into FAQs about tuberculosis, perhaps a bit of background on bovine tuberculosis (BTB) in Ireland partially provided from a 2006 article by Dr. Margaret Good of the department of agriculture would be a good start.
● September 1954- Voluntary eradication program commenced in Ireland. Britain has had a BTB program since 1935
● 1962- TB scheme became compulsory with over 170,000 reactor cattle removed
●After the start of the compulsory scheme, there was a steep drop in the number of reactors removed, but the number of reactors removed has stalled at least 30,000 reactor animals/year up until 2000
● The number of reactors removed halved in 2015 with 16,145 reactors found, but we’re still not TB free 50 years on
What is bovine tuberculosis?
Bovine tuberculosis is a disease caused by the bacteria Mycobacterium bovis. The bacteria is killed by sunlight (UV rays) but cannot be killed by drying out, and it survives in both acidic and basic environments. Reports on the length of survival of M. bovis in the environment vary from 18 to 332 days depending on temperature and sunlight exposure. The scary thing about M. bovis is that it can survive for long periods of time in warm moist areas like cattle faeces. In fact, it can survive 1-8 weeks just in cattle faeces! Bovine TB can infect a large range of mammals, though when compared to rates in cattle; it rarely infects sheep and horses. These bacteria are considered zoonotic, meaning it can infect and cause disease in people too. Typically, people contract BTB through drinking raw milk from infected cattle which is why it’s important to pasteurize milk before drinking it but farmers and those who work directly with cattle or cattle carcases are also at risk in other ways.
How do cattle get BTB?
A cow can pick up BTB many different ways, but the most common transmission scenario is when they’re exposed to another cow that is already infected. Once the bacteria get into the cow they breed and infect many different organs, primarily the lungs, digestive tract, and udder, which means that they can be expelled through breathing, infected wounds, saliva, milk, urine, and faeces. This is why testing once a year is so important. Once a cow begins shedding the bacteria it can spread through your herd very rapidly. While testing your animals every year can be costly, the loss of your whole herd would be much more devastating. Cows can also pick up the bacteria by accessing contaminated badger setts, latrines and open streams, ingesting bacteria left from an infected badger’s visit to feeding or drinking troughs, or rarely by socializing with infected deer.
What if I haven’t had a reactor in my herd for a long time?
Unfortunately that is the tricky part about BTB. Since it lives in wildlife reservoirs like badgers and to a much more limited extent deer who don’t respect fences or property lines, they can introduce BTB into your herd even after you’ve gone many years without having a reactor on your farm. Unfortunately, once it gets into a herd, BTB can spread rapidly which is why it’s so important to test yearly and cull any reactors quickly. By culling the reactor you decrease the chance that the infection will spread through the rest of your herd. But this is also why farms get locked up after a reactor has been found. It is important to do the follow up tests after the reactor has been removed, but also after the immune reaction from the first test has decreased, or else you might get false negatives or positives. This is why the two tests following the removal of a reactor must be done at least 42-days apart from one another. These follow up tests ensure other cattle that may have been socializing with the positive reactor have not become infected. Due to the slow growth of the bacteria the department has now brought in follow up tests to ensure that no cattle have become reactors since the removal of the last. Again, it may not be fun to do these tests, but it is better to test and remove than to lose a whole herd to the disease!
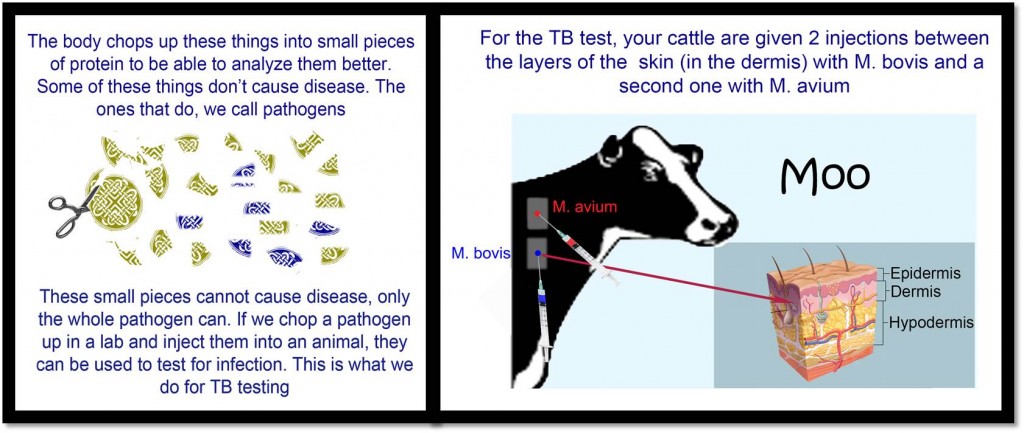
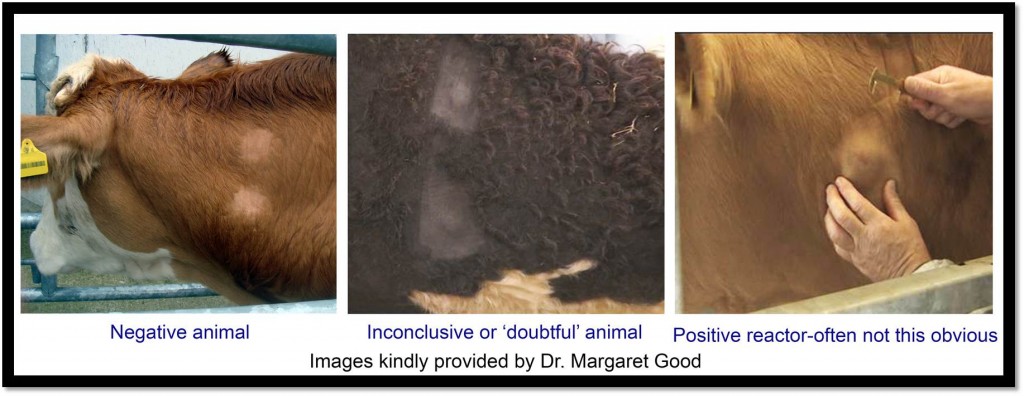
Sometimes a test will come back inconclusive and the animals are “doubtful.” In this case and especially if the animal doesn’t have TB it is important to wait before doing a follow up test because the immune response of the animal may still be overly sensitive. There are a few reasons this animal may be doubtful and not actually have TB. One reason is it may be co-infected with Johne’s disease. In this case, both of the injection sites will be raised. Another reason it might be doubtful would be that the animal was recently exposed to a similar bacteria.
What kind of information is out there on transmission from badgers and deer?
Unfortunately there isn’t too much data on transmission from deer to cattle in Ireland, but there has been a lot of data from the US where feeding stations for deer encouraged TB spread. In Ireland deer hunted for meat get examined and suspect lesions examined for TB. Only deer hunted in Wicklow have consistently shown TB lesions. In 2014, the department and IFA collaborated to look at the percent of infected deer in a small area of Wicklow with a lot of cattle TB. They found that 16% of the deer collected were infected with TB in that localised area.
TB infected badgers have been found associated with cattle infected with TB in every county in Ireland and with detailed post-mortem, up to36.3% of badgers were positive.The badger population density control program, operational since 2003, has resulted in an overall decline in mean prevalence of BTB within culled badger populations from 26% in 2007 to 11% in 2011.
What are the symptoms of Bovine Tuberculosis? How will I know if a cow has BTB?
Because of Ireland’s vigilance in testing cattle, most farmers will never see an animal showing symptoms of TB, though they begin shedding BTB before they show clinical signs. M. bovis is a very slow growing bacteria once it gets into its mammalian host, which is another reason you may not see a symptomatic animal, but they will test positive. Many reactors will never show the typical signs of a wet sounding cough, shortness of breath, swollen lymph nodes, sluggishness, and wasting away. If your cattle do show these symptoms, call a vet immediately, isolate the animal from the herd, and get it tested. While there are other diseases that can cause these symptoms, it is best to be cautious when dealing with such a nasty disease.
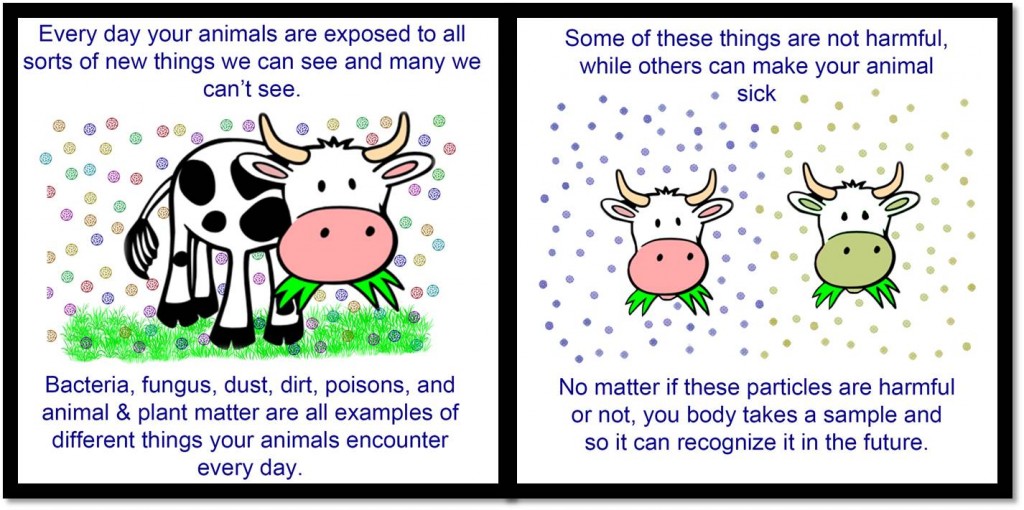
How does the TB test work?
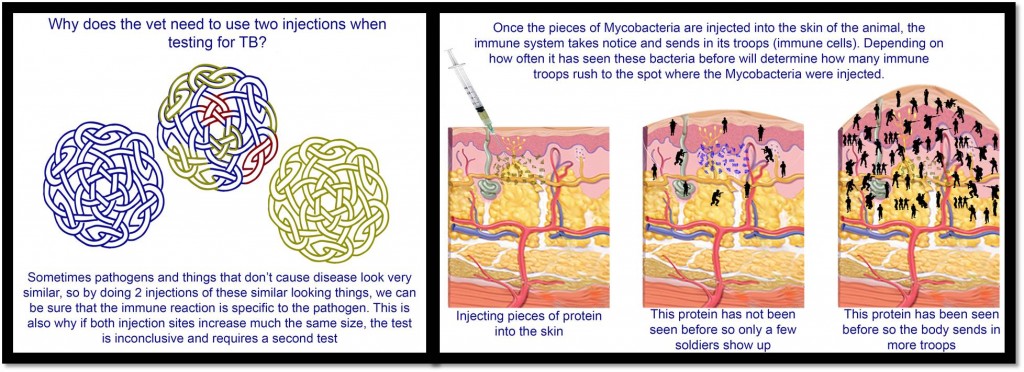
The most common TB test used in Ireland is the “Single Intradermal Comparative Tuberculin Test” (SCITT) where a vet inoculates pieces of proteins made by and from M. bovis into the skin of a cow along with proteins from a related mycobacterium, M. avium in a second site. This tests the body’s immune response to these mycobacteria. If the body has seen M. bovis before the body will rush immune cells to the site of inoculation. After the body first sees a pathogen it recognises the foreign proteins and therefore has ‘memory cells’ to combat them and quickly raise a large immune response against the proteins. The immune system is pretty good at attacking these proteins, but many proteins can be found in many different bacteria and cells, this is why vets give a second inoculation with M. avium as well. If both sites swell, then it means that the body has been exposed to some species of mycobacterium, though maybe not specifically M. bovis so a different test may need to be run to rule out M. bovis infection.
I’ve heard something about the TB test reacting with the Johne’s test. What is that about?
Johne’s disease is caused by Mycobacterium avium subspecies paratuberculosis (MAP). This means that it’s very closely related to the 2nd injection used in the TB test. As mentioned above, sometimes the immune response does not target a single specific pathogen, so if you were to look for antibodies against MAP after injecting an animal with proteins from M. bovis and M. avium, you have a very good chance of getting a false positive. This immune response can last up to 90 days after the TB test, so it is important not to test for Johne’s disease for up to 3 months after having an animal tested for TB or else you may get a false positive.
Other than culling reactors, is there anything new coming out to help us eradicate TB?
The department of agriculture has been working towards vaccination and culling strategies for badgers hoping to reduce the risk of transmission by wildlife. ICBF is taking a very different approach and actively working with department of agriculture, UCD, and Teagasc researchers to create a health index which will include BTB resistance. In 2014, Dr. Donagh Berry’s group at Teagasc along with UCD and ICBF researchers published heritabilites for BTB resistance in Irish dairy and beef cattle, and in 2016 they published data showing a location in the genome that was strongly associated with BTB resistance. This data will be critical in helping to finally eradicatebovine tuberculosis in Ireland and around the world by breeding for animals that are less susceptible to infection with M. bovis.
For more information, check out the pages on the DAFM website:
________________________________________________________________________________
I would like to say a big thank you to Dr. Margaret good for all her help and guidance on this page. Below is a list of articles that were used as sources for this material:
Abdou M. Frankena K, O’Keeffe J, Byrne AW. Effect of culling and vaccination on bovine tuberculosis infection in a European badger (Meles meles) population by spatial simulation. 2016. Preventive Veterinary Medicine. 125:19-30
Abernathy DA, Upton P, Higgins J, McGrath G, Goodchild AV, Rolfe SJ, Broughan JM, Downs SH, Clifton-Hadley R, Menzies FD, de la Rua-Domenech R, Blissitt MJ, More SJ. Bovine Tuberculosis in the UK and the Republic of Ireland, 1995-2010. 2013. Veterinary Record. doi:10.1136/vr.100969
Bermingham ML, More SJ, Good M, Cromie AR, Higgins IM, Brotherstone S, Berry DP. Genetics of Tuberculosis in Irish Holstein-Friesian dairy herds. 2009. Journal of Dairy Science. 92:3447-3456
Byrne AW, White PW, McGrath G, O’Keeffe J, Marting SW. Risk of tuberculosis cattle herd breakdowns in Ireland: effects of badger culling effort, density and historic large-scale interventions. 2014. Veterinary Research. 45:109
Good M. Bovine Tuberculosis Eradication in Ireland. 2006. Irish Veterinary Journal. 59(3):March 2006
Richardson IW, Berry DP, Wiencko HL, Higgins IM, More JS, McClure J, Lynn DJ, Bradley DG. A genome-wide association study for genetic susceptibility to Mycobacterium bovis infection in dairy cattle identifies a scusceptiblity QTL on chromosome 23. 2016. Genetic Selection and Evolution. Mar 9;48:19
Richardson IW, Bradley DG, Higgins IM, More SJ, McClure J, Berry DP. Variance component’s for susceptibility to Mycobacterium bovis infection in dairy and beef cattle. 2014. Genetic Selection and Evolution. Nov 18; 46:77
Sheridan M. Progress in tuberculosis eradication in Ireland. 2011. Veterinary Microbiology 151:160-169